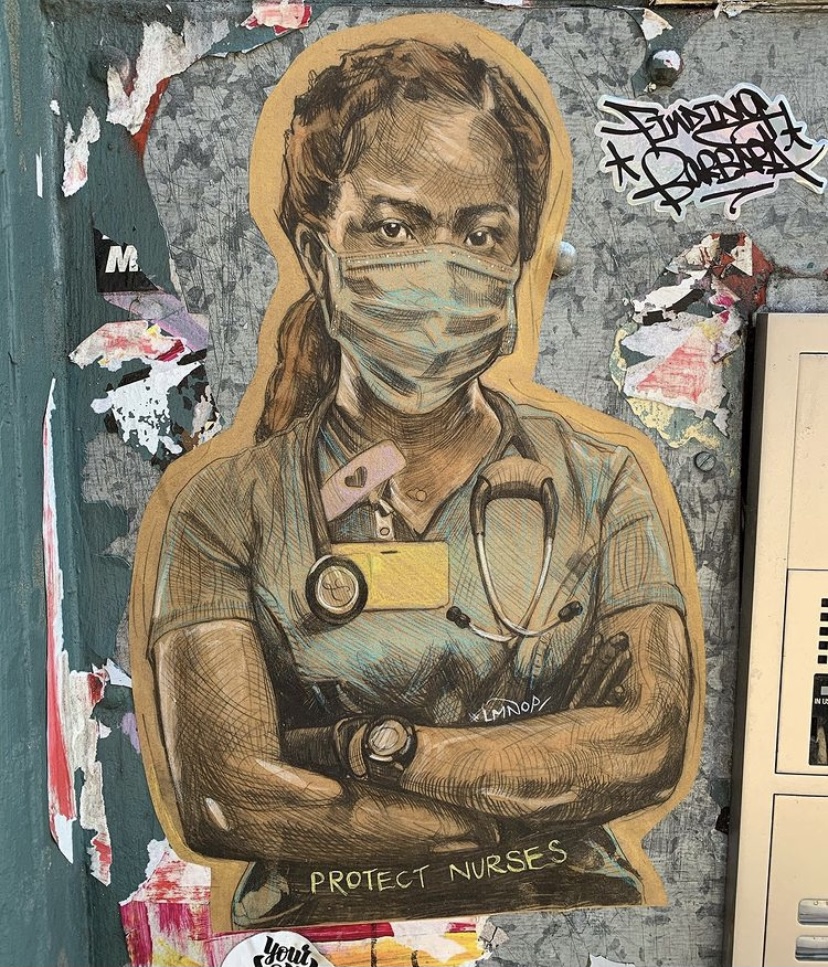
The impact of childhood trauma on pregnancy and childbirth: understanding and preventing traumatic reenactment in maternity care
When you think of childbirth you might imagine personal transformation, joy, and even empowerment. For many parents, this is true. But for individuals with a history of childhood sexual abuse (CSA), pregnancy and childbirth can kick up unwelcome reminders of past trauma. And because trauma healing is not linear, the journey to bring new life into the world can reopen old wounds.
I want to take you on a quest to explore the ways in which maternity care can reenact past abuse, even when care is provided with the best intentions. As a psychologist specializing in perinatal mental health and trauma, I have come to understand how inextricably intertwined a person’s trauma history can be with their experience of pregnancy and childbirth. Understanding this connection is critical for therapists working with women and pregnant individuals during this meaningful period of their lives.

What do you think happens when the process of childbirth itself—the intimate procedures, the potential for perceived loss of control, the encounters with strangers—feels hauntingly similar to the past experiences of abuse? The answer can be found in a qualitative study conducted by Montgomery et al. (2015), where the experiences of nine women who had been sexually abused as children were analyzed to understand how maternity care can unintentionally mirror past abuse. Despite efforts to provide sensitive care, the study found that certain aspects of childbirth can still replicate aspects of past sexual abuse.
One of the most striking findings of this study was the role of intrusive medical procedures on triggering memories of abuse. For women who had been sexually abused, vaginal examinations—a necessary part of maternity care—could evoke feelings of violation and fear, even when the procedure was done with care. For example, one participant in the study shared that she felt violated during a routine examination, linking it directly to her childhood experiences.
What do you think happens when the process of childbirth itself—the intimate procedures, the potential for perceived loss of control, the encounters with strangers—feels hauntingly similar to the past experiences of abuse?
Pain is an inevitable reality of childbirth, and for women with a history of CSA, labor pain can disturbingly overlap with the emotional and physical pain they experienced during past traumatic events. In the study, several women described how the anticipated and experienced pain of childbirth transported them back to their abuse. One woman expressed fear that her childhood trauma memories would “get into her head” before she gave birth. Another participant reported finding herself unable to breathe during labor and delivery; a response that she later connected to her childhood abuse. In the throes of labor, her body remembered what her mind could not consciously hold. This research suggests that, for sexual trauma survivors, pain management in childbirth is not just about physical relief; it is about creating a space where they can feel safe and in control of their bodies.

It comes as no surprise that control is a central theme in both trauma and childbirth. For sexual abuse survivors, the legacy of their trauma often centers around the loss of control over their bodies. In childbirth, this loss of control can be re-experienced, particularly when medical interventions become necessary. Even pregnancy itself can make expectant parents feel disempowered. One of the participants in the study described feeling like the “baby was taking over” her body. Her words echo the experience of many trauma survivors who feel as though their bodies are once again being controlled by an external force during pregnancy. This loss of agency, combined with the medicalization of maternal healthcare and childbirth, can destabilize the expectant parent.
These research findings highlight why working with survivors during pregnancy requires a clear understanding of their trauma history and a sensitivity to how medical interventions can inadvertently trigger a trauma response. Trauma-informed providers and therapists alike must recognize how the body can remember past trauma. Even when the rational mind knows that a medical procedure is distinct from abuse, the body can respond as if it is the same.
In the throes of labor, her body remembered what her mind could not consciously hold.
What can be done to protect CSA survivors from re-experiencing trauma during pregnancy and childbirth? Building trust between healthcare providers and women with a history of CSA is essential. Montgomery et al. (2015) emphasizes the importance of creating a safe, respectful environment where women feel in control of their care. This might mean allowing them to make decisions about how procedures are conducted or ensuring continuity of care so that they can build a trusting relationship with their provider. Therapists working with pregnant women and individuals can prepare their clients for how pregnancy and childbirth might bring up traumatic memories and equip them with resources to navigate childbirth effectively. Therapists can also help women advocate for themselves during pregnancy and childbirth. They can support them in articulating their needs, setting boundaries, and ensuring that they feel empowered throughout the process. Trauma-informed care is not just about avoiding triggers; it’s about creating an environment where women feel safe, respected, and empowered.
If you’re a provider interested in learning more about birth trauma and recovery, I encourage you to take my Birth Trauma Recovery Training. Together, we can create a community of trauma therapists dedicated to supporting women through one of the most meaningful experiences of their lives.
References:
Montgomery, E., Pope, C., & Rogers, J. (2015). The re-enactment of childhood sexual abuse in maternity care: A qualitative study. BMC Pregnancy and Childbirth, 15, 194. https://doi.org/10.1186/s12884-015-0626-9